Understanding HPV and Abnormal Pap Smears
Human Papillomavirus (HPV) is a widely prevalent virus that is passed from person to person through skin-to-skin contact. Although these strains are spread through sexual contact, sexual intercourse is not necessary to spread HPV. It may be spread through any sexual contact. It has been suggested that about three out of four sexually active people may have a genital HPV infection at some point in their lives.
There are over 120 known strains of HPV at present and only about 15 of those strains are linked to cervical cancer, and approximately 12 strains may cause genital warts. For women over 30, a pap smear checks for any abnormal cells as well as detectable strains of high risk HPV. In women under 30, high risk HPV is tested only if the pap smear reveals any abnormal cells. This is because cervical cancer is very rare under the age of 30 and most women with HPV are able to clear the virus on their own. Adolescents have an almost 80% clearance rate for high risk HPV.
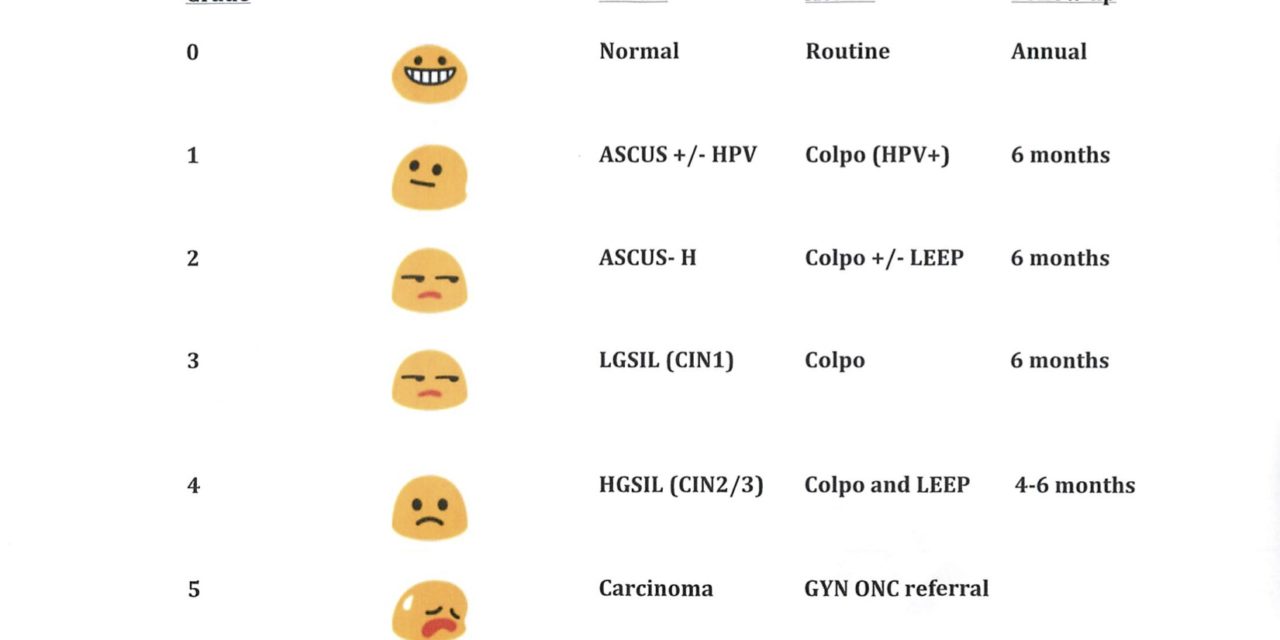
Abnormal pap results may be reported as “Abnormal cells of unknown significance (ASCUS)” , low grade intra-epithelial lesion ( LGSIL) or high grade squamous intra-epithelial lesion ( HGSIL). The next steps in care are decided depending on the results of the pap smear. If you are positive for HR HPV ( high risk human papilloma virus) and don’t have any abnormal cells, you may just need to be watched closely for any cell changes. You will be advised to have a test called colposcopy which includes examination of cervix under magnification and a cervical biopsy ( sampling). Depending on the results, you may need 6 monthly follow up or removal of abnormal cells by a small procedure called LEEP or cryofreezing. It is important to remember that testing positive for HPV does not mean that you have cervical cancer.
HPV affects men as well as women. HPV testing is currently not widely prevalent for males. Therefore, it may be hard to go back and figure out who the high risk HPV infection was contracted from. HPV can survive and lay dormant (asleep) inside the cervical cells for many years before detection. Condoms may help prevent HPV transmission, but HPV can also infect areas that are not covered by a condom, therefore they may not prevent complete transmission.
The current recommendations for prevention against high risk HPV infection include HPV quadrivalent vaccination. There are two such vaccines available. The quadrivalent ( effective against 4 strains) is Gardasil vaccine. The Gardasil vaccine is recommended for females and males ages 9-26. Gardasil offers protection against 4 strains of HPV (6, 11, 16 &18) which account for 75% of cervical cancer cases (strains 16&18) and 90% of genital wart cases (strains 6&11). The injection is given in a 3 shot series over 6 months. The vaccine has minimal, if any, side effects. Most insurances cover the vaccination series. The vaccination can be offered or prescribed by your gynecologist or pediatrician.
For any additional questions or to schedule the Gardasil vaccination, please feel free to walk in or call us as Walk IN GYN Care ( walkingyn.com).


Recent Comments